Does Medicaid Cover Braces for All Ages?
If you’re wondering if Medicaid covers braces, the answer will likely depend on various factors such as age, medical necessity, and where you live. This article breaks down the conditions under which Medicaid might cover braces, helping you understand the requirements and navigate the application process efficiently.
Key Takeaways
- Medicaid will likely provide orthodontic coverage for individuals under 21 and may offer limited coverage for adults when it’s medically necessary, with certain states determining specific eligibility and scope of services.
- Medicaid’s criteria for braces coverage will likely focus on medical necessity – including improvement of oral health, chewing, or speech – and generally prioritize patients under 21, with exceptions for adults in medically necessary cases.
- The potential coverage and application process for Medicaid orthodontic services may vary by state, and seeking an orthodontist who accepts Medicaid might involve online directories and non-profit resources for affordable care.
Compare Plans in One Step!
Enter Zip Code
Understanding Medicaid and Orthodontic Coverage
Medicaid is a government healthcare program that has been designed to provide affordable health coverage to:
- low-income adults
- children
- elderly individuals
- individuals with disabilities
Its goal will likely be to ensure that these individuals can access to the healthcare they need, including dental benefits. It could provide a lifeline for these individuals, possibly providing extensive coverage for various medical services, such as orthodontic treatment.

Orthodontic treatment, particularly for children, could form a significant part of what Medicaid might offer. Medicaid will likely cover braces to improve dental health. Dental braces could serve a dual purpose, as they could align teeth and play a critical role in rectifying bite and tooth alignment, which could hold significant importance for long-term oral health.
What is Medicaid?
Medicaid is a government healthcare program that could provide extensive medical coverage to individuals with low incomes. It might not directly administer healthcare but instead relies on private managed care plans to cover their beneficiaries. Medicaid will likely reimburse healthcare providers, such as hospitals and doctors, for the services provided to eligible patients.
The Medicaid program has been jointly funded by the federal and state governments, with the federal government providing a specified percentage of the program costs. Medicaid coverage may also encompass a wide range of healthcare services, which might include:
- Inpatient and outpatient hospital services
- Physician services
- Laboratory and x-ray services
- Home health services
- Early and periodic screening, diagnostic, and treatment services
Orthodontic Treatment and Medicaid
Braces and other orthodontic treatments could be a significant investment. Luckily, Medicaid may provide coverage for orthodontic treatment based on orthodontic and financial needs.
Medicare will likely offer coverage for braces for children who are under the age of 21 through the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefits, which may also include emergency dental services.
For adults, Medicaid might provide coverage for orthodontic services only when considered medically necessary, such as in cases of severe misalignment of the teeth that could impair essential functions. Keep in mind that Medicaid will likely not cover braces for purely cosmetic reasons.
Medicaid’s Criteria for Braces Coverage
Medicaid has established certain guidelines for braces coverage. Firstly, braces may be deemed medically necessary by Medicaid when they are used to treat or prevent a condition, injury, or symptoms that could impact oral health, chewing, or speech. Braces may be deemed medically necessary if they are utilized to:
- Reposition teeth for improved chewing function
- Make bite adjustments for treating temporomandibular joint disorders
- Prevent sleep apnea caused by teeth restricting airflow
Secondly, there may be age restrictions in place. Medicaid will likely offer coverage for braces that have been restricted to individuals who are under the age of 21. However, exceptions could be made if the braces have been deemed medically necessary for adults.
Medical Necessity
The concept of ‘medical necessity’ will likely be a key determinant in assessing eligibility for Medicaid’s orthodontic coverage. States may define ‘medical necessity’ for braces as the treatment of a malocclusion that might compromise the individual’s health.

Conditions that may indicate ‘medical necessity’ for braces under Medicaid include functional impairment, restoration of optimal chewing function, and correction of bite issues. To establish ‘medical necessity,’ the documentation required may encompass additional dental records, X-rays, or letters from healthcare providers that could elucidate the medical necessity of orthodontic treatment.
Age Requirements
The age of the patient could be a major factor in Medicaid’s coverage of braces. Medicaid orthodontic coverage will likely be accessible for children and adolescents below the age of 21, provided that it has been considered medically necessary. The Children’s Health Insurance Program (CHIP), under Medicaid, may also extend coverage to children under 19 years of age.
Children might receive more extensive coverage compared to adults, especially due to the Children’s Health Insurance Program (CHIP). Although Medicaid could offer coverage for adults, the coverage for children, particularly under the children’s health insurance program, may be broadened by the Affordable Care Act to potentially encompass more services.
Orthodontic Services Covered by Medicaid
Medicaid will likely cover a variety of orthodontic services, which might include:
- Removable appliance therapy
- Fixed appliance therapy
- Interceptive orthodontic treatment
- Comprehensive orthodontic treatment
The coverage for each of these treatments under Medicaid may vary by state, so it’s important to check if your state’s Medicaid coverage could include the specific treatment you need.
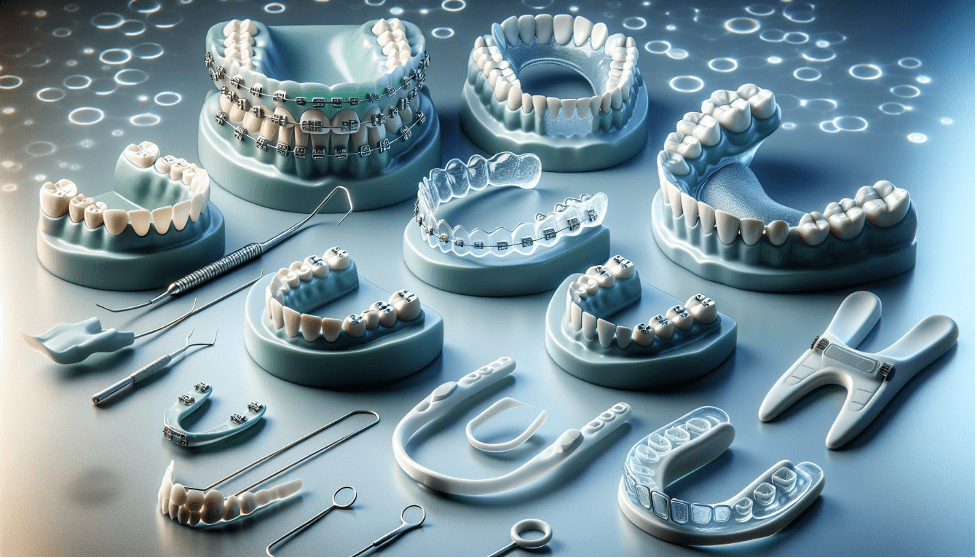
For example, fixed appliance therapy might encompass the use of traditional orthodontic braces to address more intricate dental concerns. On the other hand, removable appliance therapy will likely involve the use of removable devices, such as retainers or aligners, to address minor orthodontic issues.
Removable Appliance Therapy (D8210)
Removable appliance therapy in orthodontics may also encompass the utilization of removable orthodontic appliances, also referred to as removable orthodontic retainers. These appliances may be commonly employed for addressing single-tooth rotations and could be specifically structured to prevent the teeth from undergoing misalignment once again.
Orthodontic conditions that may be amenable to treatment through removable appliance therapy might include:
- Overbite
- Gaps
- Teeth crowding
- Open occlusion
- Overjet
- Deep malocclusion
- Posterior crossbite
Fixed Appliance Therapy (D8220)
Fixed appliance therapy (D8220) will likely involve treatments such as traditional metal braces utilized for the realignment of teeth. These treatments might be covered under Medicaid. Fixed appliance therapy may also be employed to correct more intricate dental concerns and could also be used to manage habits like thumb sucking or tongue thrusting.
The coverage for D8220 under Medicaid may differ by state, so it is important to examine the potential benefits and eligibility criteria that could be specific to each state’s Medicaid program for fixed appliance therapy.
Interceptive Orthodontic Treatment (D8060)
Interceptive orthodontic treatment will likely involve early interventions in orthodontics to prevent or minimize the severity of future dental malocclusions. Medicaid may also include coverage for this form of treatment as part of its range of orthodontic services for eligible beneficiaries.
Interceptive orthodontic treatment (D8060) may also aim to prevent or potentially minimize the necessity for comprehensive treatment by intervening early in a developing issue. This could encompass the use of appliances such as space maintainers, palatal expanders, or limited braces.
Comprehensive Orthodontic Treatment (D8080)
Comprehensive orthodontic treatment (D8080) might encompass the initial six months of treatment, final records, photos, and panoramic x-rays. This could be specifically tailored to adolescent dentition, which may address the teenage years when permanent teeth have fully erupted.
Comprehensive orthodontic treatment may also aim to address dental and skeletal irregularities in adolescent dentition. Some of the procedures that might be encompassed in this treatment may include:
- Expanders
- Partial fixed appliance
- Headgear
- Re-evaluation
State-Specific Medicaid Coverage for Braces
As the Medicaid coverage for braces might not be uniform across all states, understanding the differences in eligibility criteria and covered services becomes important. While some states might offer potential benefits for orthodontic treatment, others may provide limited coverage.
To ascertain if your state’s Medicaid program might include coverage for braces, you could reach out to your Medicaid caseworker or the state health department for the most accurate information.
State-by-State Comparison
The differences in Medicaid policies for braces across different states will likely be attributed to various coverage options and eligibility criteria. This variability may be contingent upon the individual rules and funding of each state’s Medicaid program.
The age requirements for Medicaid braces coverage will likely prioritize individuals aged 21 and below, although there may be variations in specific criteria across different states. Some states may provide coverage for these services, while others may only offer them in cases of medical necessity.
Finding Your State’s Medicaid Information
To comprehend the specific coverage options and eligibility criteria for braces, it may be important to find your state’s Medicaid information.
Understanding state-specific Medicaid information could be vital due to each state’s authority to determine its coverage options for orthodontic treatment. To gain insight into the potential orthodontic coverage in a particular state, it may be crucial to review the state’s Medicaid information.
Resources and databases such as the State Resource Center and Medicaid & CHIP Open Data site could aid in comprehending state-specific Medicaid information.
Applying for Medicaid Orthodontic Coverage
There may be several steps involved in applying for Medicaid coverage for orthodontic treatment. Firstly, you might need to obtain an evaluation by a certified orthodontist to verify the necessity for braces.
For adults, it could be essential to demonstrate that braces represent the most economical and effective method to address a non-dental health issue.
After the orthodontist validates the need for braces, you may need to prove the cost-effectiveness of the treatment. Here are the steps to establish cost-effectiveness for Medicaid:
- Analyze the potential costs of orthodontic treatment.
- Identify the possible factors that could influence the price.
- Explore potential affordable payment plans.
- Assess the overall cost-effectiveness of the treatment for Medicaid.
Assessment by an Orthodontist
An orthodontic assessment will likely play a key role in evaluating the eligibility for Medicaid coverage of braces. During the assessment, an orthodontic scoring system could be utilized to evaluate the severity of the orthodontic condition. Potential factors such as:
- oral hygiene
- dental check-ups
- cavity status
- the extent of the orthodontic condition
should be taken into consideration by orthodontists during Medicaid’s orthodontic assessment.
To be eligible for Medicaid coverage, the orthodontic provider must submit the following:
- A completed copy of the HLD Index
- Accompanying documentation to verify the score by dental
- Additional documentation such as a medical diagnosis and surgical treatment plan
- Detailed documentation of extenuating circumstances
- Detailed documentation from a mental health professional
These documents will likely be necessary to verify eligibility for Medicaid coverage.
Demonstrating Cost-Effectiveness
The demonstration of cost-effectiveness may also be important for Medicaid orthodontic coverage. This could allow Medicaid programs to offer adult coverage for viable preventive dental procedures, which might improve oral health outcomes and potentially reduce healthcare costs.
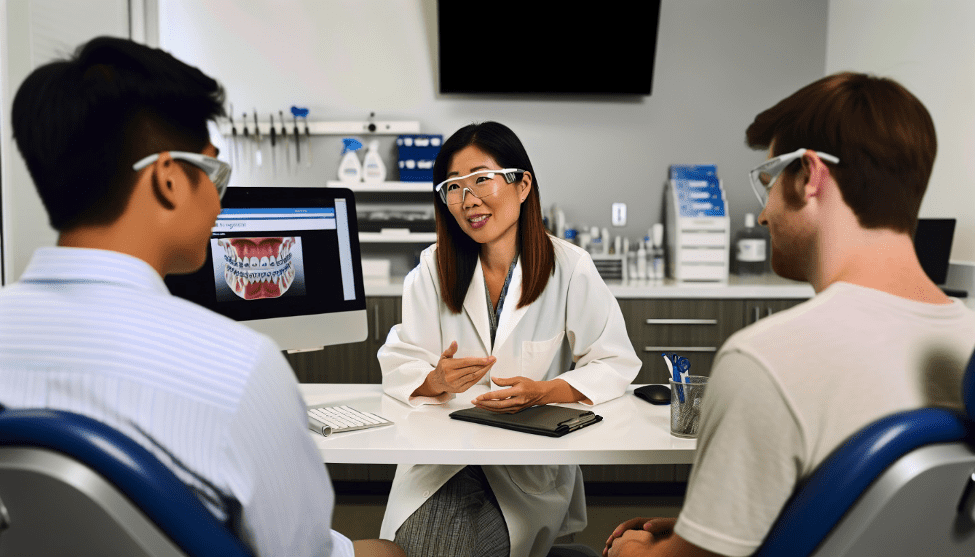
Cost-effectiveness in the realm of orthodontic treatment will likely involve the assessment of the intervention with the resources utilized. Reimbursement for orthodontic treatment for Medicaid may be contingent upon orthodontic and financial needs, and the criteria will likely be determined by Medicaid.
Finding an Orthodontist Who Accepts Medicaid
Locating an orthodontist who accepts Medicaid might seem challenging. However, online directories such as Zocdoc or organizations like Kool Smiles could help locate orthodontists who accept Medicaid.
Certain orthodontists may also offer a complimentary consultation for Medicaid beneficiaries, although the availability of this service may differ, so it will likely be advisable to inquire directly with the orthodontic office.
Possible Limitations and Exceptions to Medicaid Coverage
Despite Medicaid being a lifeline for many for orthodontic treatment, understanding its potential limitations and exceptions is important. Medicaid might have limitations on both the duration and scope of orthodontic treatment coverage, which may be limited to individuals under the age of 21.
Exceptions could be made if the braces have been deemed medically necessary for adults. As for the frequency of Medicaid-covered orthodontic visits, it has been recommended to have 1 visit every 6 months for oral health screening or assessment.
Alternative Options for Affordable Orthodontic Care
In case Medicaid coverage is unavailable or inadequate, other affordable options for orthodontic care exist. Certain nonprofit organizations such as the Smile for a Lifetime Foundation and Smiles Change Lives could potentially offer affordable orthodontic care to individuals in need.
Some dental payment plans may also ease the financial burden of orthodontic treatments by potentially enabling patients to spread the cost through manageable installments.
Other potential cost-effective alternatives for orthodontic treatment might encompass options such as:
- Retainers
- Traditional metal braces
- Ceramic braces
- Clear aligners
Summary
Medicaid could be a valuable resource for individuals in need of orthodontic treatment. While the coverage might vary by state and certain restrictions may apply, these plans could provide a lifeline for many, particularly children under 21.
It’s essential to understand the specific coverage options and eligibility criteria in your state and to find an orthodontist who accepts Medicaid. If Medicaid coverage is not available or insufficient, there may be alternative options for affordable orthodontic care.
Frequently Asked Questions
→ How to get Texas Medicaid to pay for braces?
To get Texas Medicaid to pay for braces, the member must have a severe handicapping malocclusion or special medical conditions such as cleft palate or skeletal anomalies involving the oral cavity. These will likely be the conditions for which comprehensive orthodontic services may be covered by Texas Medicaid.
→ Does Medicare cover braces?
Medicare might cover orthodontic care only if it has been deemed medically necessary, such as for severe misalignment impacting your health. Cosmetic orthodontic care will likely not be covered, unless you have a Medicare Advantage plan with that specific benefit.
→ Does Medicaid pay for braces in SC?
Yes, Medicaid in South Carolina will likely cover =braces for children if they have been medically necessary under the EPSDT benefit.
→ Does Medicaid cover braces in New York?
No, Medicaid in New York may only cover braces for children under 21 with severe physically handicapping malocclusions, for a limited period of time.
→ What is the objective of Medicaid’s coverage for orthodontic treatment?
The objective of Medicaid’s coverage for orthodontic treatment will likely be to enhance dental health for eligible individuals.

ZRN Health & Financial Services, LLC, a Texas limited liability company
Russell Noga is the CEO of ZRN Health & Financial Services, and head content editor of several Medicare insurance online publications. He has over 15 years of experience as a licensed Medicare insurance broker helping Medicare beneficiaries learn about Medicare, Medicare Advantage Plans, Medigap insurance, and Medicare Part D prescription drug plans.



