Medicare Advantage Plans Alabama 2026
Looking into the potential Medicare Advantage Plans in Alabama
Key Takeaways
- Medicare Advantage Plans in Alabama include a range of options such as HMO, PPO, and Special Needs Plans (SNPs), each catering to varying healthcare needs and preferences.
- Some Medicare Advantage plans may offer additional benefits that could go beyond Original Medicare, including dental, vision, and hearing coverage, possibly making them a comprehensive healthcare choice.
- Enrollment periods, including Initial Enrollment, Annual Enrollment, and Open Enrollment, are crucial for beneficiaries to understand in order to manage their healthcare coverage effectively.
Compare Plans in One Step!
Enter Zip Code
Understanding Medicare Advantage Plans Alabama 2026
Medicare Advantage Plans, offered by private insurance companies, could provide an alternative to Original Medicare. Some plans may integrate additional services, such as prescription drug coverage, dental, vision, and hearing coverage. Medicare Advantage Plans in Alabama will likely be designed to offer robust support for managing healthcare needs through comprehensive offerings.
Types of Medicare Advantage Plans Available
Alabama Medicare Advantage plans will likely offer a diverse range of plans that could cater to different healthcare needs and preferences. These include Health Maintenance Organization (HMO) plans, Preferred Provider Organization (PPO) plans, and Special Needs Plans (SNPs). Each type of plan has its unique features and benefits, ensuring that there is an option to suit every individual’s situation.
HMO Plans
HMO plans are designed to provide coordinated care through a network of healthcare providers. Members are required to select a primary care physician (PCP) who manages their overall healthcare. To see specialists or receive certain services, members typically need referrals from their PCP. This structure could help ensure that care is well-coordinated and that patients receive the necessary preventive services.
One of the potential advantages of HMO plans might be that they cover in-network services, except in emergencies. This could potentially lead to more predictable costs for members. HMO plans may also include worldwide emergency and urgent care coverage, providing peace of mind for members who travel.
PPO Plans
For those seeking greater flexibility, PPO plans allow members to see any doctor or specialist without needing a referral. This means you could choose your healthcare providers more freely, although using in-network providers might result in lower costs. This flexibility may be ideal for individuals who prefer to have more control over their healthcare decisions.
PPO plans might come with higher out-of-pocket costs for out-of-network services compared to in-network ones. However, the flexibility could make them a comprehensive choice for many beneficiaries.
Special Needs Plans (SNPs)
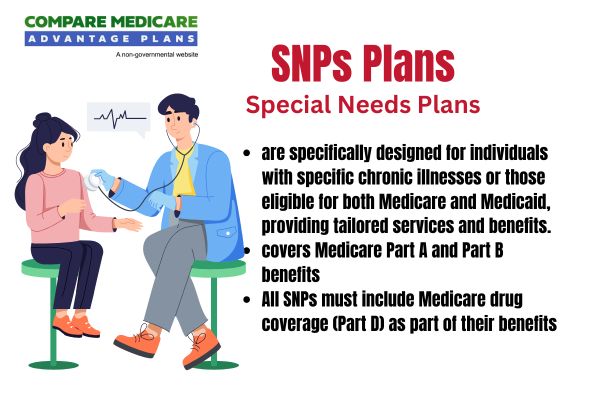
Special Needs Plans (SNPs) are tailored for individuals with specific health requirements, such as chronic conditions or disabilities, and those who are dual-eligible for Medicare and Medicaid. These plans provide specialized benefits and care coordination to meet the unique needs of their members.
There are three types of SNPs: Dual-Eligible Special Needs Plans (D-SNPs), Chronic Condition Special Needs Plans (C-SNPs), and Institutional Special Needs Plans (I-SNPs). Each plan could address the specific challenges faced by its members, possibly ensuring they receive the comprehensive care and support they need.
Overview of Medicare Advantage Plans in Alabama 2026
As we approach
Potential Benefits of Alabama Medicare Advantage Plans 2026

Some Medicare Advantage plans may offer a variety of additional benefits, such as dental, vision, and hearing coverage, which are not typically included in Original Medicare.
Certain plans may also feature lower out-of-pocket expenses compared to traditional Medicare, possibly offering a cost-effective choice for beneficiaries. This comprehensive approach could potentially ensure that members receive the necessary care to maintain their health and well-being, as the comprehensive coverage they offer.
Enrollment Process for Alabama Medicare Advantage Plans
Enrolling in Medicare Advantage plans involves understanding the specific enrollment periods and taking timely action. Whether you are enrolling for the first time or switching plans due to discontinuation, it’s crucial to be aware of the dates and deadlines to ensure uninterrupted coverage.
The following sections will provide detailed information on the various enrollment periods and the steps to enroll.
When to Enroll
The Annual Enrollment Period (AEP) for Medicare Advantage plans begins on October 15 each year. This period allows individuals to review and select new plans for the upcoming year. For those turning 65, there is a seven-month window surrounding their birthday during which they can enroll in a Medicare Advantage plan. To ensure coverage starting in January, individuals must enroll by December 31.

If your current plan is being discontinued, you have options. You can utilize the Special Enrollment Period from December 8 to February 28 each year. This period allows affected members to switch to a new plan without any lapse in coverage. Acting within these enrollment windows ensures uninterrupted healthcare benefits.
Different Enrollment Periods
There are multiple enrollment windows that beneficiaries need to be aware of. Besides the Annual Enrollment Period, there is the Initial Enrollment Period, which lasts seven months, starting three months before turning 65, including the birthday month, and extending three months after. This beginning period is crucial for those new to Medicare.
There is also the Medicare Advantage Open Enrollment Period, which takes place from January 1 to March 31. This period allows individuals already enrolled in a Medicare Advantage plan to switch or return to Original Medicare.
Additionally, Special Enrollment Periods (SEPs) enable beneficiaries to change their plans due to specific life events, such as moving or losing health coverage.
OEP, AEP, Special Enrollment
The Annual Enrollment Period (AEP), occurring from October 15 to December 7, allows beneficiaries to make changes to their Medicare plans. This is a critical time for reviewing and selecting the best options for your healthcare needs.
The Open Enrollment Period (OEP) runs from January 1 to March 31, providing an opportunity to switch Medicare Advantage plans or revert to Original Medicare. For those experiencing significant life events, the Special Enrollment Period (SEP) allows for plan changes outside the usual enrollment windows, ensuring continuous coverage.
Potential Costs Associated with Alabama Medicare Advantage Plans 2026
Understanding the cost structure of Medicare Advantage plans will likely be essential for making an informed decision. Some plans may involve a combination of premiums, co-pays, and an out-of-pocket maximum.
The following subsections will delve into these cost components in detail.
Premiums and Co-Pays
The premiums and co-pays for Medicare Advantage plans may vary significantly based on the specific plan selected. Some plans might offer lower premiums compared to Original Medicare, possibly making them an attractive option for those looking to minimize monthly expenses.
Members should also understand the difference between co-payments and coinsurance, where co-pays are fixed amounts paid for covered services, and coinsurance is a percentage of the cost that the member pays. Being aware of these details could help you manage your healthcare budget more effectively.
Out-of-Pocket Maximums
Some Medicare Advantage plans may offer an out-of-pocket maximum, which could potentially cap the total amount you will pay for covered services each year. This could potentially provide significant financial protection against high medical costs. However, the limit might vary depending on the specific plan chosen.
This potential safeguard could ensure that once you reach your plan’s maximum limit, you won’t have to pay for additional covered healthcare services for the rest of the year, possibly providing peace of mind and financial predictability.
How to Qualify for Alabama Medicare Advantage Plans 2026
To qualify for Medicare Advantage plans in 2025, individuals must enroll in a new plan by December 31 if their current plan is discontinued. Enrollment opens on October 15, during the Annual Enrollment Period. This timing is crucial to ensure continuous coverage.

Eligibility criteria include being enrolled in Medicare Part A and Part B and residing in the service area of the plan you wish to join. Special Enrollment Periods are available for certain life events, allowing for flexibility in enrollment.
Providing required personal health information ensures you receive suitable coverage based on your medical needs upon request.
Contracted Network and Access to Care
Medicare Advantage plans offer access to a network of healthcare providers, including specialists and hospitals, likely ensuring coordinated care. For HMO plans, a primary care provider typically coordinates member care within the contracted network. This network structure could help manage costs and likely ensures that members receive consistent, high-quality care.
Members may also seek care from out-of-network providers, but the costs might be higher compared to in-network services. Medicare Advantage Plans in Alabama also incorporate worldwide emergency and urgent care coverage, providing peace of mind for travelers.
Comparing Alabama Medicare Advantage Plans to Original Medicare
Medicare Advantage plans, unlike Original Medicare, are offered by private insurance companies and some may provide additional benefits not covered by Original Medicare. These might include dental, vision, and hearing services, as well as prescription drug coverage.
The following subsections will delve into the specific coverage differences and cost comparisons between these plans.
Coverage Differences
Some Medicare Advantage plans may offer a broader range of benefits compared to Original Medicare. Certain plans may include additional benefits such as dental, hearing, and vision coverage, which are not typically offered by Original Medicare.
Certain plans may also incorporate prescription drug coverage, whereas Original Medicare requires a separate Part D plan. Additionally, some plans might have an out-of-pocket maximum limit, potentially offering financial protection against high medical costs.
Cost Comparisons
In terms of cost, some Medicare Advantage plans may offer lower out-of-pocket expenses compared to Original Medicare, depending on the specific plan and coverage options selected. This could make these plans a cost-effective choice for many beneficiaries.
Medicare Advantage plans might feature annual out-of-pocket maximums, possibly providing financial protection by capping the total expenses for covered services. This cap is absent in Original Medicare, which could lead to higher out-of-pocket costs.
Emergencies and Referrals

Medicare Advantage HMO plans often require members to receive referrals from their primary care provider (PCP) before seeing specialists. This likely ensures that care is well-coordinated. However, in the case of emergencies, Medicare Advantage plans cover urgent care and emergency room visits without needing prior authorization, providing immediate access to necessary care.
For non-emergency situations, Medicare Advantage plans may require referrals to see specialists, but this might vary by plan type. Additionally, plans typically cover emergency services worldwide, allowing members to seek care without prior authorization or referrals, ensuring they are protected no matter where they are.
Summary
Medicare Advantage plans in Alabama will likely offer a comprehensive and flexible alternative to Original Medicare, with a potential variety of benefits and services designed to meet diverse healthcare needs. Understanding the different types of plans, enrollment periods, possible costs, and coverage options is crucial for making informed decisions. As you navigate the options
Frequently Asked Questions
→ When can I enroll in a new Medicare Advantage plan?
You can enroll in a new Medicare Advantage plan during the Annual Enrollment Period, which runs from October 15 to December 31 each year. Make sure to mark your calendar for these important dates.
→ What additional benefits could Medicare Advantage plans offer?
Some Medicare Advantage plans may offer additional benefits such as dental, vision, and hearing services. These potential benefits could contribute to a more comprehensive healthcare experience.
→ What is the out-of-pocket maximum for Medicare Advantage plans?
The plan details
→ How do Medicare Advantage plans might compare to Original Medicare in terms of cost?
Some Medicare Advantage plans may offer lower out-of-pocket costs and sometimes additional benefits that are not covered by Original Medicare. Therefore, these plans could be a cost-effective option for many beneficiaries.

ZRN Health & Financial Services, LLC, a Texas limited liability company