Understanding Medicare Advantage Plans
Medicare Advantage plans, also known as Part C, offer a comprehensive alternative to traditional Medicare. These plans typically encompass coverage for hospital care, medical services, and often prescription drugs. Provided by private insurance companies approved by Medicare, they offer a unique blend of benefits tailored to meet diverse healthcare needs.
One of the standout features of Medicare Advantage plans is the additional benefits they provide, which are not available through Original Medicare. These can include dental, vision, and even wellness programs, enhancing overall coverage and ensuring a more holistic approach to healthcare. Additionally, exploring medicare supplement plans can further enhance your healthcare options.
Most plans require members to use a network of doctors and hospitals for non-emergency care, making it crucial to consider provider networks, plan choices, and the plan’s network when selecting a plan.
Key Factors to Consider When Comparing Plans in 2026
When comparing Medicare Advantage plans in 2026, consider the following steps:
- Start with a thorough review of the medications and healthcare services you regularly use to identify which plans offer the best coverage for your specific needs.
- Take time to compare options costs, benefits, and the quality of plans.
- Utilize online comparison tools to streamline the process, allowing you to filter options effectively and find the plan that best suits your needs.
Provider networks play a significant role in determining if your preferred pharmacies, doctors, and hospitals are covered under the plan. Having these other providers in-network can minimize out-of-pocket costs and provide easier access to the care you need.
Additionally, many Medicare Advantage plans provide free preventive care services, which can help keep you healthy and save money on medical expenses in the long run. Medicare plans can also offer various benefits to support your health.
Provider Networks and Access
Choosing a Medicare Advantage plan with an extensive provider network can significantly influence your access to preferred healthcare services. Consider the following:
- Check if your preferred providers are part of the plan’s network.
- Be aware that plans with limited networks may require you to travel further for care.
- Understand that limited networks may lead to higher costs for out-of-network services.
Out-of-pocket costs can be minimized by ensuring that a plan’s network includes your preferred doctors and hospitals. When selecting a Medicare Advantage plan, consider the following:
- Different plans may have varying provider networks, affecting accessibility for enrollees.
- Potential restrictions on referrals for specialty services.
- Prior authorizations required for specialty services.
Medicare Advantage PPOs
Medicare Advantage PPOs offer flexibility and freedom in choosing healthcare providers:
- Unlike HMOs, PPO plans allow beneficiaries to see any Medicare-approved provider without needing referrals.
- Using out-of-network services typically incurs higher costs.
- This flexibility is particularly beneficial for those who travel frequently or have provider preferences that extend beyond a specific network.
PPO plans often include prescription drug coverage as part of their benefits, allowing members to receive comprehensive care without needing separate drug plans. However, it’s important to note that while PPOs provide greater provider access, they generally come with higher out-of-pocket costs when using out-of-network providers.
Emergency and urgent care services are typically covered regardless of the provider’s network status, ensuring access to necessary care when it matters most.
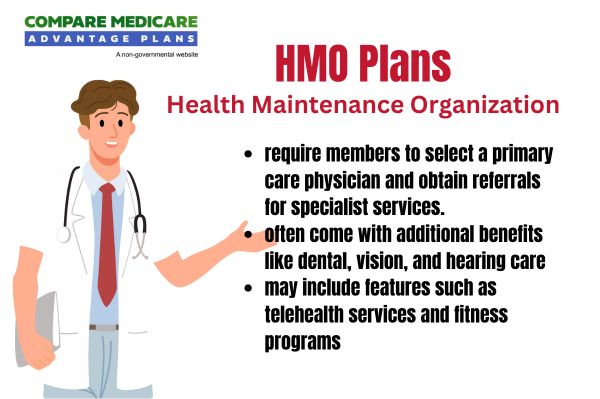
Medicare Advantage HMOs
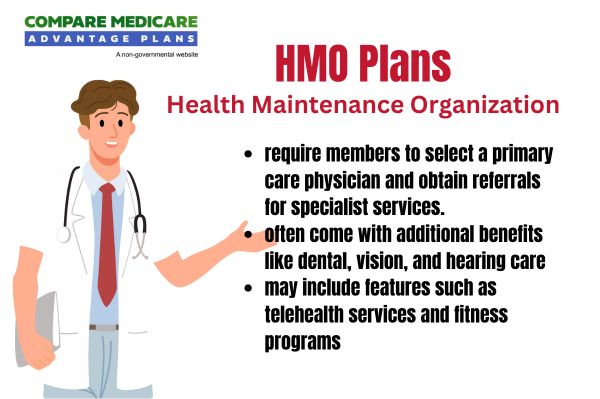
Medicare Advantage HMOs are known for:
- Lower premiums
- Comprehensive coverage options
- Requirement for members to use a network of doctors and hospitals, which helps keep costs down but can limit provider access compared to PPOs
- Additional benefits like dental and vision coverage, which are not available in traditional Medicare
In 2024, enrollment in Medicare Advantage plans, including HMOs, reached over 32.8 million people enrolled, surpassing half of the Medicare-eligible population. These plans must provide a maximum out-of-pocket limit, offering financial protection that traditional Medicare does not. HMOs also employ cost management tools, such as prior authorization requirements, to control spending and ensure efficient use of resources.
Prescription Drug Coverage
Prescription drug coverage is a critical component of most Medicare Advantage plans. Understanding the level of drug coverage provided by each prescription drug plan is important since it can differ widely. Reviewing the formulary of Medicare Part D prescription drug plans ensures that your prescription drugs are covered, helping to avoid unexpected expenses. Additionally, considering various prescription drug plans can help you find the best option for your needs.
In 2026, out-of-pocket spending on covered Part D drugs will reach a threshold of $2,100, capping prescription drug costs. Once the d deductible for Part D drugs of up to $615 is met, a 25% coinsurance applies to subsequent costs. This structure helps manage prescription costs and provides financial predictability for Medicare beneficiaries through cost sharing.
Costs and Premiums
Projected changes in Medicare premiums for 2026 include:
- Medicare Advantage plans: average monthly premiums are expected to decrease by approximately 14%, making these plans more affordable for many beneficiaries.
- Standalone Part D plans: the average premium is anticipated to fall to about $34.50.
- Part B premium: set to rise from $185 to $206.50 monthly.
Different plans may have varying out-of-pocket expenses for medical services, which can significantly impact overall medical costs. Medicare Advantage plans have out-of-pocket limits, capping annual out-of-pocket costs and providing financial protection.
The catastrophic threshold for Part D, which acts similarly to an out-of-pocket maximum, will increase from $2,000 to $2,100.