Beyond the standard coverage, Blue Cross HMO Blue Advantage Plans offer a variety of extra benefits that significantly enhance the healthcare experience. These additional benefits include:
- Dental
- Vision
- Hearing
- Over-the-counter (OTC) allowances
- Telehealth services
- Fitness programs
These benefits provide greater access to essential covered services and contribute to better overall health management for members, resulting in valuable rewards as an independent licensee. This is a sign of progress in our approach.
These extra benefits underscore the comprehensive nature of the Blue Cross HMO Advantage Plans. By including such a broad range of services, the plans ensure that members have access to all the tools they need to maintain and improve their health. This holistic approach to healthcare sets these plans apart, offering value beyond standard Medicare offerings.
Prescription Drug Coverage

Members of the Anthem Medicare Advantage HMO plans benefit from extensive prescription drug coverage, including programs for managing complex medication needs. This comprehensive coverage ensures that members have access to necessary medications without the burden of high out-of-pocket costs, as provided by the medicare advantage organization.
Many Medicare Advantage HMO plans offer prescription drug coverage with no deductibles on certain tiers. This feature simplifies access to medications and reduces financial stress. By providing comprehensive prescription drug coverage, Blue Cross HMO Advantage Plans ensure that members can manage their health effectively and affordably.
Vision and Hearing Aids
The Blue Cross HMO Advantage Plan includes comprehensive vision care coverage, ensuring members receive essential eye care. Members are eligible for:
- Routine eye exams
- Coverage for glasses
- Coverage for contact lenses This makes it easier for members to maintain their vision health without incurring high costs.
The plan also offers coverage for hearing aids, addressing the auditory needs of members effectively. Incorporating both vision and hearing aid benefits emphasizes the Blue Cross HMO Advantage Plan’s commitment to holistic member health. These benefits help members maintain their sensory health, contributing to a better quality of life.
Wellness Programs
Preventive services included in Medicare Advantage plans cover various tests and screenings, along with routine vaccinations. Anthem offers a fitness program named SilverSneakers, which is often included in their Medicare Advantage plans. This program encourages physical activity, contributing to overall health and well-being.
The Blue Cross HMO Advantage Plans often provide additional perks like transportation for medical appointments and allowances for over-the-counter health items. These wellness programs enhance the healthcare experience by offering services that promote health maintenance and disease prevention. Incorporating such initiatives ensures members can lead healthier, more active lives.
Eligibility and Enrollment
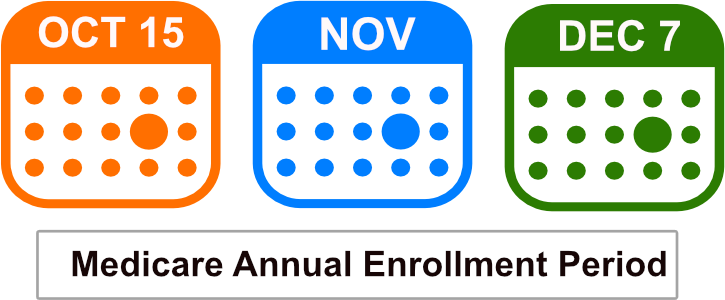
Eligibility and enrollment are critical aspects of Medicare Advantage Plans. During the annual enrollment period, members can evaluate their options and switch plans if desired. This flexibility allows individuals to choose the plan that best meets their changing healthcare needs.
The Initial Enrollment Period for Medicare Advantage begins three months before turning 65 and ends three months after. Special Enrollment Periods also allow enrollment outside of the standard times based on personal life changes. Knowing these enrollment periods is essential for timely access to healthcare benefits.
Eligibility Requirements
To enroll in Medicare Advantage Plans, individuals must meet specific eligibility requirements. The Initial Enrollment Period starts three months before the 65th birthday and ends three months after. This period is crucial for new enrollees to secure their benefits without delay.
Special Enrollment Periods allow individuals to enroll outside the standard times due to personal life changes such as moving or losing other health coverage. These provisions ensure that individuals can maintain continuous healthcare coverage during significant life transitions. Knowing these eligibility requirements helps prospective members plan their enrollment effectively.
Enrollment Process
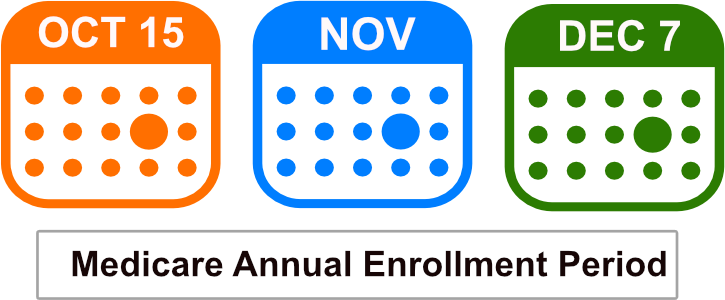
The Annual Enrollment Period for making changes to Medicare Advantage plans occurs yearly from October 15 to December 7. During this time, individuals can make changes to their plans, ensuring they have the best coverage for their needs in the coming year.
To enroll, members must participate by following specific steps, including reviewing plan options, comparing benefits, and completing the necessary paperwork. This process ensures that members are fully informed and can make the best decisions for their healthcare needs.
Understanding the enrollment process enables members to fully benefit from Blue Cross HMO Advantage Plans.
Claims and Customer Support
Submitting claims and accessing customer support are vital components of managing your healthcare plan. Claims can be submitted electronically through a third-party clearinghouse for faster processing, ensuring that members receive timely reimbursements. For paper claims, using the correct forms, such as CMS-1500 for professional claims or UB-04 for institutional claims, is essential.
To check the status of a claim, members can contact customer support for updates on receipt and adjudication. The BlueCard program allows members to submit claims for services received outside their home area, ensuring continuous coverage. By understanding how to navigate claims and customer support, members can manage their healthcare expenses more effectively.
Contract Renewal and Changes
Understanding contract renewal and potential changes is crucial for members of Blue Cross HMO Advantage Plans. Enrollment in these plans generally occurs during specific periods each year, and it is contingent on whether the medicare contract with Medicare is still active. Annual contract renewals for Anthem Medicare Advantage plans depend on agreements with the Centers for Medicare & Medicaid Services (CMS). This ensures that the plans remain compliant with regulatory standards and continue to offer up-to-date benefits.
Members receive notifications regarding any changes to their plans before the start of the new plan year. These changes can include updates to coverage for services, enhanced benefits, additional coverage, or modified cost-sharing structures.
Anthem may adjust benefits or premiums during the renewal period based on regulatory changes or market conditions. Understanding these potential changes helps members make informed decisions about their healthcare coverage.